Finding a new normal
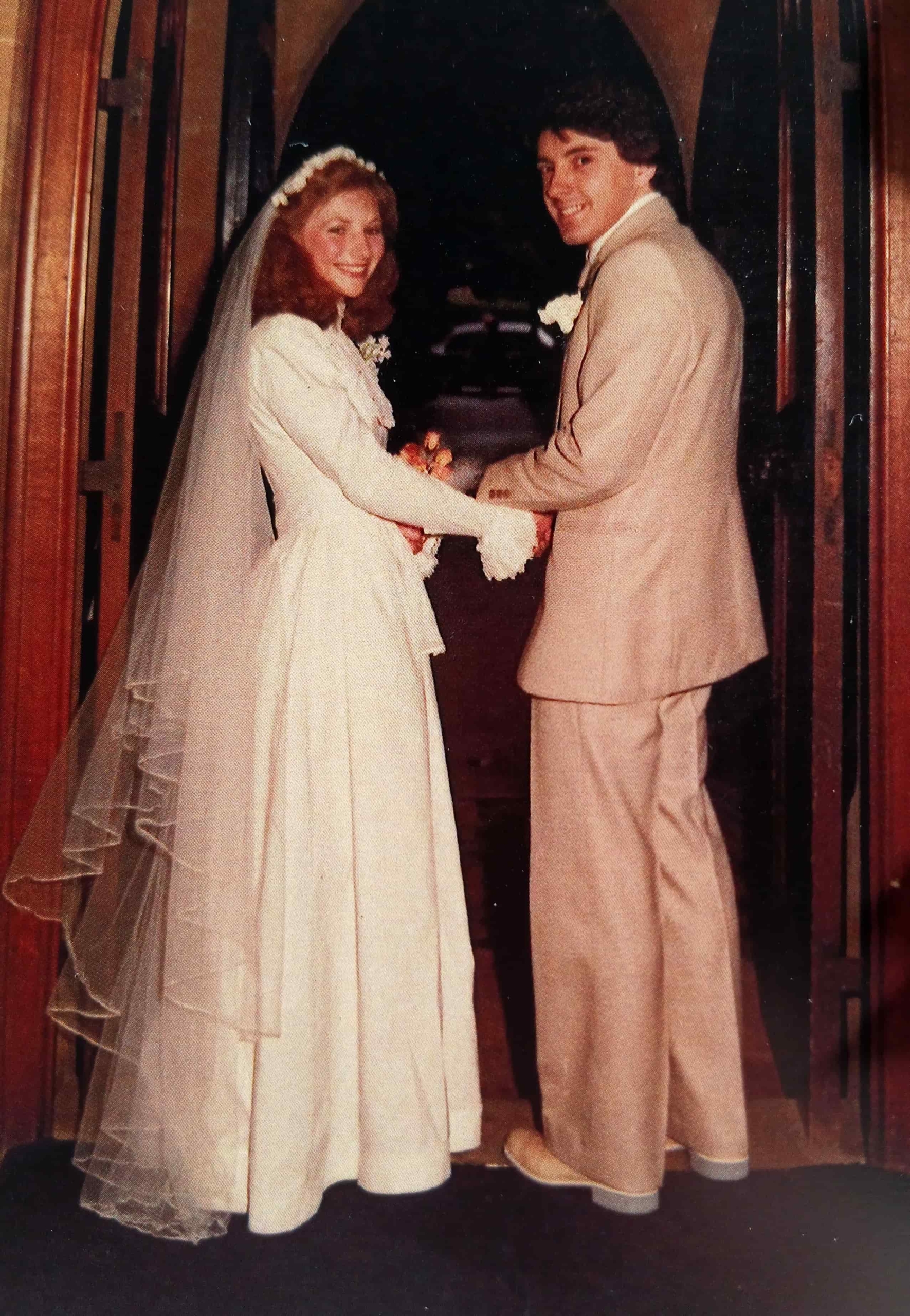
When Sarah* lost her husband Alex in April this year, just weeks before their 45th wedding anniversary, she was faced with the complicated reality of life without the person she had spent nearly all her adult years alongside.
Their dementia journey began in 2018 when Alex experienced a sudden and severe headache, leading to the discovery of a brain bleed. Over the next several years, these bleeds became more frequent – sometimes four in a year – caused by cerebral amyloid angiopathy, a condition that makes blood vessels in the brain fragile and prone to rupture.
Some bleeds left little lasting effect. Others robbed Alex of his speech, mobility, or memory. Recovery was possible, but it took daily rehabilitation, speech therapy, and constant vigilance.
Living with uncertainty
Sarah remembers the shock of the first time a doctor used the word ‘dementia,’ a diagnosis that added another layer of complexity to Alex’s care.
“We were at the stroke clinic, and I was concerned about his memory. I said, ‘Do you think he’s got dementia?’ and the doctor said, ‘Oh yes, he’s got vascular dementia’ – like I should have already known. But no one had ever mentioned that.”
From then on, life was lived on high alert. “I was living on eggshells a lot of the time,” she says. “A normal day could turn into a medical emergency in an instant – in the garden, at home, or even while shopping.”
Living with that uncertainty also meant making some difficult but necessary decisions. Very early on, Sarah and Alex updated their wills and arranged Enduring Powers of Attorney. It wasn’t easy to have those conversations, but she’s grateful now that everything was clearly documented.
Balancing care and daily life
Support was limited. Monthly dementia group meetings through Dementia Auckland offered genuine connection and understanding from others that truly understood, but family help wasn’t always available. For Sarah, these groups became a lifeline.
“It was a safe place where you could be vulnerable and know people understood, without feeling judged,” she says.
Sharing experiences helped ease feelings of guilt and showed her she wasn’t alone. The groups also provided practical advice, tips, and information — and the reassurance that others were going through similar, or sometimes even harder, situations.
Sarah also chose to return to part-time work during this time — a decision that gave her some structure and focus beyond her caring role, while still balancing the demands of supporting Alex.
Over time, Alex’s needs grew. His judgment and decision-making began to change, leading to safety concerns. An incident just before Christmas, when he became disoriented while travelling by bus, made it clear he could no longer be out alone.
His personality also shifted. At times, he could be impatient or unsettled, waking in the early hours and getting dressed for the day. For Sarah, it was a gradual grieving process – losing the husband she had known long before his physical death.
“It all became so hard,” she reflects. “He wasn’t the person I’d married. It was a horrendous time.”
When care needs change
In March this year, Alex was admitted to hospital again, a few weeks before Sarah herself was due for surgery. Because she would be unable to care for Alex during that period, a needs assessment was carried out, and it was concluded that Alex required hospital-level care.
While a nursing home was being sought, Alex began to wander from the ward, sometimes into other patients’ rooms and the needs assessment was upgraded to dementia-level care. Sarah recalls feeling the weight of the situation – managing her own pressing health needs while navigating a care system already under pressure and a husband with chronic health needs.
Life after loss
Alex unexpectedly passed away in April. Since then, Sarah has been overwhelmed with the practical realities that follow loss: legal matters, finances, and day-to-day decisions she once shared. It’s an unfamiliar process, full of forms, deadlines, and unexpected tasks that seem to keep appearing just when she feels she’s making progress.
“You think you’ve sorted one thing, and then something else comes up that you’ve never had to deal with before,” she says.
She also feels like part of her is missing – the person she was with him. “It’s about trying to rebuild a life, but I’m not quite ready for that.”
In the weeks that followed Alex’s death, Sarah found herself doing things she hadn’t had the time or energy for before – like taking her first long bath in years.
“It sounds small, but it felt like a milestone,” she says. “Now I’m trying to notice those little things, like enjoying a cup of tea without rushing, or having a quiet moment to myself.”
For now, she’s taking each day as it comes. She’s grateful for the moments they shared before his death, even when they were challenging.
“You don’t realise how much you’ll miss the little things – the conversations, the routines – until they’re gone.”
Sarah hopes her story encourages other care partners to seek support early, to find people who understand, and to know they don’t have to face the journey alone.
What Sarah describes – the constant vigilance, the gradual loss, the mixed emotions after a loved one’s passing – will feel familiar to many care partners. Her honesty gives space for those feelings, whatever they may be, to simply exist.
Our Dementia New Zealand Network is here to help care partners and whānau navigate their own ‘new normal’ after a dementia diagnosis – reach out to a Dementia Advisor if you’d like to chat.
* Names have been changed to protect privacy
Dementia Auckland create safe, understanding spaces for care partners and whānau across the city. But demand is growing. Right now, Dementia Auckland supports over 2100 families every month, and the number of people needing help is expected to rise by more than 140% in the next 25 years.
With your support, we can ensure that every family has access to the same understanding and practical advice that made such a difference for Sarah.